Guidance History
| Date | Description of Change |
|---|---|
| 3/13/2020 | Original guidance issued |
| 5/28/2020 | Language added to clarify the compliance date to cease reporting to TYPE-OF-CLAIM value “Z” as June 2021 |
| 8/30/2023 | Language added to clarify reporting of CLAIM-LINE-STATUS in relation to the header status. Language concerning subcapitation payments was removed as all relevant instructions may be found in a separate T-MSIS Coding Blog entry. |
Brief Issue Description
Multiple states are unclear what constitutes a denied claim or a denied encounter record and how these transactions should be reported on T-MSIS claim files.
Background Discussion
Context
Reason Why CMS Wants States to Submit Denied Claims and Encounters
CMS needs denied claims and encounter records to support CMS’ efforts to combat Medicaid provider fraud, waste and abuse. The data are also needed to compute certain Healthcare Effectiveness Data and Information Set (HEDIS) measures. If a claim was submitted for a given medical service, a record of that service should be preserved in T-MSIS. It does not matter if the resulting claim or encounter was paid or denied.
For additional background, readers may want to review Appendix P.01: Submitting Adjustment Claims to T-MSIS in the T-MSIS Data Dictionary, version 2.3.
Definitions
FFS Claim – An invoice for services or goods rendered by a provider or supplier to a beneficiary and presented by the provider, supplier, or his/her/its representative directly to the state (or an administrative services only claims processing vendor) for reimbursement because the service is not (or is at least not known at the time to be) covered under a managed care arrangement under the authority of 42 CFR 438.
Managed Care Encounter Claim – A claim that was covered under a managed care arrangement under the authority of 42 CFR 438 and therefore not paid on a fee-for-service basis directly by the state (or an administrative services only claims processing vendor). Encounter records often (though not always) begin as fee-for-service claims paid by a managed care organization or subcontractor, which are then repackaged and submitted to the state as encounter records.
Adjudication – The process of determining if a claim should be paid based on the services rendered, the patient’s covered benefits, and the provider’s authority to render the services. Claims for which the adjudication process has been temporarily put on hold (e.g., awaiting additional information, correction) are considered “suspended” and, therefore, are not “fully adjudicated.”1
Denied FFS Claim2 – A claim that has been fully adjudicated and for which the payer entity has determined that it is not responsible for making payment because the claim (or service on the claim) did not meet coverage criteria. Examples of why a claim might be denied:
- Services are non-covered
- Beneficiary’s coverage was terminated prior to the date of service
- The patient is not a Medicaid/CHIP beneficiary3
- Services or goods have been determined not to be medically necessary
- Referral was required, but there is no referral on file
- Required prior authorization or precertification was not obtained
- Claim filing deadline missed
- Invalid provider (e.g., not authorized to provide the services rendered, sanctioned provider)
- Provider failed to respond to requests for supporting information (e.g., medical records)
- Missing or Invalid Service Codes (CPT, HCPCS, Revenue Codes, etc.) which have not been provided after the payer has made a follow-up request for the information
The complete list of codes for reporting the reasons for denials can be found in the X12 Claim Adjustment Reason Code set, referenced in the in the Health Care Claim Payment/Advice (835) Consolidated Guide, and available from the Washington Publishing Company.
Denied Managed Care Encounter Claim – An encounter claim that documents the services or goods actually rendered by the provider/supplier to the beneficiary, but for which the managed care plan or a sub-contracted entity responsible for reimbursing the provider/supplier has determined that it has no payment responsibility.
Challenges
Contractual Scenarios and Their Impacts on the Creation of Denied Claim or Encounter Records
The contractual relationships among the parties in a state’s Medicaid/CHIP healthcare system’s service delivery chain can be complex. For example, the Medicaid/CHIP agency may choose to build and administer its provider network itself through simple fee-for-service contractual arrangements. In such an arrangement, the agency evaluates each claim and determines the appropriateness of all aspects of the patient/provider interaction. Alternatively, the Medicaid/CHIP agency may choose to contract with one or more managed care organizations (MCOs) to manage the care of its beneficiaries and administer the delivery-of and payments-for rendered services and goods. The agency may contract with the prime MCO on a capitated basis, but then the MCO might choose to build its provider network by: subcontracting with other MCOs on a FFS basis or capitated basis, subcontracting with individual providers on a FFS basis or capitated basis, and/or with some other arrangements. Additionally, the structure of the service delivery chain is not limited to a two- or three-level hierarchy.
While the pay/deny decision is initially made by the payer with whom the provider has a direct provider/payer relationship, and the initial payer’s decision will generally remain unchanged as the encounter record moves up the service delivery chain, the entity at every layer has an opportunity to evaluate the utilization record and decide on the appropriateness of the underlying beneficiary/provider interaction. Whenever it concludes that the interaction was inappropriate, it can deny the claim or encounter record in part or in its entirety and push the transaction back down the hierarchy to be re-adjudicated (or voided and re-billed to a non-Medicaid/CHIP payer). At each level, the responding entity can attempt to recoup its cost if it chooses. If the recoupment4 takes the form of a re-adjudicated, adjusted FFS claim, the adjusted claim transaction will flow back through the hierarchy and be associated with the original transaction. If the denial results in the rendering provider (or his/her/its agent) choosing to pursue a non-Medicaid/CHIP payer, the provider will void the original claim/encounter submitted to Medicaid.
Regardless of the number of levels of subcontracts in the service delivery chain, it is not necessary for the state to report the pay/deny decision made at each level. The state should report the pay/deny decision passed to it by the prime MCO. This process is illustrated in Diagrams A & B.
Diagram A: Decision Tree for Reporting Managed Care Encounter Claims – Provider/Initial Payer Interactions
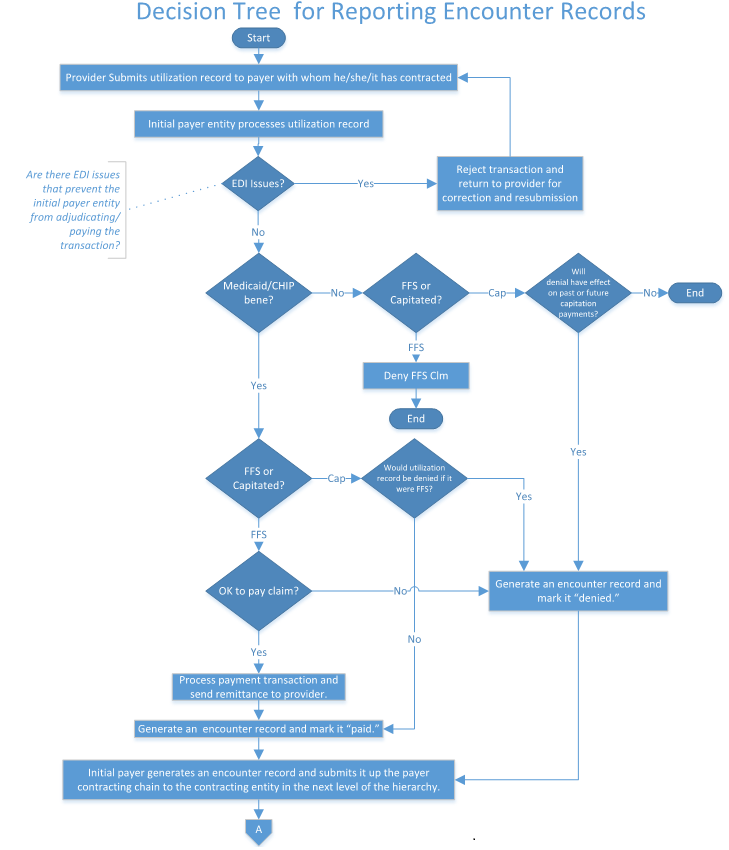
Diagram B: Decision Tree for Reporting Encounter Records – Interactions Among the MCOs Comprising the Service Delivery Hierarchy

CMS Guidance
- All claims or encounters that complete the adjudication/payment process should be reported to T-MSIS. This is true even if the managed care organization paid for services that should not have been covered by Medicaid. See Diagram C for the T-MSIS reporting decision tree.

- Suspended claims (i.e., claims where the adjudication process has been temporarily put on hold) should not be reported in T-MSIS. Additionally, claims that were rejected prior to beginning the adjudication process because they failed to meet basic claim processing standards should not be reported in T-MSIS. NOTE: Transactions that fail to process because they do not meet the payer’s data standards represent utilization that needs to be reported to T-MSIS, and as such, the issues preventing these transactions from being fully adjudicated/paid need to be corrected and re-submitted.
- All denials (except for the scenario called out in CMS guidance item # 1) must be communicated to the Medicaid/CHIP agency, regardless of the denying entity’s level in the healthcare system’s service delivery chain. It will not be necessary, however, for the state to identify the specific MCO entity and its level in the delivery chain when reporting denied claims/encounters to T-MSIS. Simply reporting that the encounter was denied will be sufficient.
- Voids and Adjustments of previously denied claims or encounter records must be communicated to the Medicaid/CHIP agency (except for the scenario called out in CMS guidance item # 1), so that the Medicaid/CHIP agency can include the information in its T-MSIS files.
- The Medicaid/CHIP agency must report changes in the costs related to previously denied claims or encounter records whenever they directly affect the cost of the Medicaid/CHIP program. Depending on the nature of the payment arrangements among the entities of the Medicaid/CHIP healthcare system’s service supply chain, these may take the form of voided claims (or encounters), adjusted claims (or encounters), or financial transactions in the T-MSIS files.
- Whenever an entity denies a claim or encounter record, it must communicate the appropriate reason code up the service delivery chain.
- The Medicaid/CHIP agency must include the claim adjustment reason code that documents why the claim/encounter is denied, regardless of what entity in the Medicaid/CHIP healthcare system’s service supply chain made the decision. This code should be reported in the ADJUSTMENT-REASON-CODE data element on the T-MSIS claim file.
- To the extent that it is the state’s policy to consider a person “in spenddown mode” to be a Medicaid/CHIP beneficiary, claims and encounter records for the beneficiary must be reported T-MSIS.
Instructions for Populating Data Elements Related to Denied Claims or Denied Claim Lines.
States’ MMIS systems may flag denied claims (or denied claim lines) differently from one another. Regardless of how a state identifies denied claims or denied claim lines in its internal systems, the state should follow the guidelines below to identify denied claims or denied claim lines in its T-MSIS files.
CLAIM-DENIED-INDICATOR – If the entire claim is denied, the CLAIM-DENIED-INDICATOR should be set to “0”. If some, but not all, of the lines on the claim transaction are denied, the CLAIM-DENIED-INDICATOR should be set to “1”. If none of the lines on the claim transaction are denied, the CLAIM-DENIED-INDICATOR should be set to “1”. The CLAIM-DENIED-INDICATOR set to “0” is the way that T-MSIS data users will identify completely denied claim transactions.
CLAIM-LINE-STATUS – If a particular detail line on a claim transaction is denied, its CLAIM-LINE-STATUS code should be one of the following values: “542”, “585”, or “654”. Any other value will be interpreted as indicating a paid line. If all of the lines on a claim transaction are denied, then the CLAIM-DENIED-INDICATOR should be set to “0”, rather than setting each line’s CLAIM-LINE-STATUS to one of the denied code values (“542”, “585”, or “654”).- If the header is paid (e.g., CLAIM-DENIED-INDICATOR = 1), then at least one claim line must be paid (i.e., CLAIM-LINE-STATUS <> 542, 585, or 654).
- If all lines are denied (i.e., CLAIM-LINE-STATUS = 542, 585, or 654), then the header must be denied (e.g., CLAIM-DENIED-INDICATOR = 0).
CLAIM-STATUS – Logically speaking, if the CLAIM-DENIED-INDICATOR equals “0” (the entire claim is denied), one would expect the CLAIM-STATUS code data element to equal one of the following values: “542” (Claim Total Denied Charge Amount), “585” (Denied Charge or Non-covered Charge), or “654” (Total Denied Charge Amount).
An inconsistency between the CLAIM-DENIED-INDICATOR value and the CLAIM-STATUS value will trigger a validation edit error.
Please note, however, that T-MSIS data users will use CLAIM-DENIED-INDICATOR equals “0” to identify a completely denied claim transaction, regardless of the CLAIM-STATUS value reported on the claim transaction’s header record.
CLAIM-STATUS-CATEGORY – Logically speaking, if the CLAIM-DENIED-INDICATOR equals “0” (the entire claim is denied), one would expect the CLAIM-STATUS-CATEGORY value to equal “F2” (Finalized/Denial-The claim/line has been denied).
An inconsistency between the CLAIM-DENIED-INDICATOR value and the CLAIM-STATUS-CATEGORY value will trigger a validation edit error.
As is the case with CLAIM-STATUS, however, T-MSIS data users will use CLAIM-DENIED-INDICATOR equals “0” to identify a completely denied claim transaction, regardless of the CLAIM-STATUS-CATEGORY value reported on the claim transaction’s header record.
TYPE-OF-CLAIM – TYPE-OF-CLAIM value “Z” should not be used.
Use of the TYPE-OF-CLAIM value “Z” will trigger a validation edit error.
States will be required to cease reporting to value “Z” by June 2021. After that point, any files not corrected may be required to be resubmitted.
The TYPE-OF-CLAIM code should be the code that would have been used if the claims were paid.
[1] Suspended claims are not synonymous with denied claims. The responsibility-for-payment decision has not yet been made with regard to suspended claims, whereas it has been made on denied claims. Suspended claims should not be reported to T-MSIS. NOTE: Paid encounters that do not meet the state’s data standards represent utilization that needs to be reported to T-MSIS. EDI issues preventing these transactions from being fully adjudicated/paid need to be corrected and re-submitted to the Payer.
[2] A denied claim and a zero-dollar-paid claim are not the same thing. While both would have $0.00 Medicaid Paid Amounts, a denied claim is one where the payer is not responsible for making payment, whereas a zero-dollar-paid claim is one where the payer has responsibility for payment, but for which it has determined that no payment is warranted. (Examples include: previous overpayments offset the liability; COB rules result in no liability.)
[3] If the payer entity determines during the adjudication process that it has no payment responsibility because the patient is not a Medicaid/CHIP beneficiary, it is not necessary for the state to submit the denied claim to T-MSIS. However, if the payer initially makes payment and then subsequently determines that the beneficiary is not a Medicaid/CHIP beneficiary, then CMS expects the claim to be reported to T-MSIS (as well as any subsequent recoupments). (See footnote #4 for a definition of “recoupment.”)
[4]“Recoupment” means:
- Recoveries of overpayments made on claims or encounters.
- TPL recoveries that offset expenditures for claims or encounters for which the state has, or will, request Federal reimbursement under Title XIX or Title XXI.
- Rebates that offset expenditures for claims or encounters for which the state has, or will, request Federal reimbursement under Title XIX or Title XXI.

