Managed Care Quality Improvement
As the dominant delivery system for Medicaid and the Children's Health Insurance Program (CHIP), managed care has enormous potential to achieve state priorities and improve health care quality and outcomes. Federal regulations at 42 CFR 438 subpart E (Quality Measurement and Improvement) require states with managed care contracts to carry out a set of managed care quality (MCQ) oversight activities, which include developing and updating state quality strategies (QS), establishing and implementing the state’s ongoing quality assessment and performance improvement (QAPI) programs, and conducting external quality review (EQR) activities. QAPI programs include performance measures and performance improvement projects (PIPs).
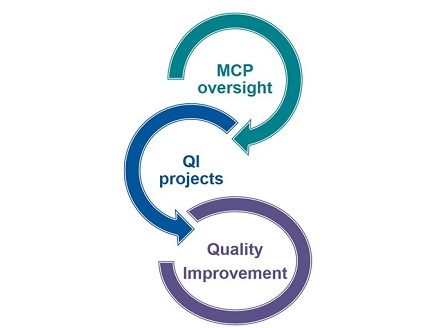
These activities inform and reinforce each other as shown in the “MCQ Cycle” below. States should update their MCQ oversight documents regularly, incorporating lessons learned from each one into the others and into quality improvement (QI) projects.
Learn more about:
MCQ Cycle

The Cycle includes the MCQ oversight activities that support oversight and QI in managed care, including QS, QAPI programs, and EQR, each feeding into and reinforcing the others.
Using MCQ Oversight Activities to Support QI Projects
States can use the MCQ oversight activities to support QI projects and to ensure that QI projects align with the state’s managed care QI priorities.

Use Quality Strategies to:
- Identify focus areas for QI projects
- Inform the development of QI project aim statements and selection of change ideas
- Video: Using State Managed Care Quality Strategies for QI in Medicaid and CHIP

Use External Quality Reviews to:
- Review managed care plan level findings and identify managed care plans to work with or populations to focus on
- Identify promising QI project change ideas to test
- Video: Using Managed Care External Quality Review for QI in Medicaid and CHIP

Use managed care Quality Assessment and Performance Improvement programs to:
- Identify measures for QI project measurement strategies
- Identify learnings from performance improvement projects
- Sustain and spread successful QI project ideas
- NEW: Webinar: Quality Improvement in Medicaid and CHIP Managed Care: Quality Assessment and Performance Improvement (QAPI) Programs
States’ QI projects can inform MCQ oversight:
- States can refine their QS goals and objectives to reflect aims from successful QI projects or large upcoming QI initiatives.
- States can test QI project change ideas or spread successful change ideas by adding targeted QAPI PIPs to their managed care plan contracts.
- As an optional EQR activity under 42 CFR §438.358(c), states can ask their EQROs to calculate measures included in a QI project measurement strategy to help assess the QI project’s impact at the managed care plan or program level.
Technical Assistance Resources
The Centers for Medicare & Medicaid Services (CMS) has developed a variety of resources to support states seeking to expand the reach and impact of QI by aligning MCQ oversight activities and QI projects in their Medicaid and CHIP managed care programs.
- Fact Sheet: Medicaid and CHIP Managed Care Quality Improvement. This June 2024 fact sheet summarizes the MCQ cycle and describes opportunities to align the MCQ cycle with other Medicaid and CHIP quality oversight and improvement efforts.
- Webinar: Using Medicaid and CHIP Managed Care Quality Oversight Activities for Quality Improvement (audio, transcript). This July 2023 webinar describes how MCQ oversight activities—QS, EQR, and QAPI—are interconnected and how state Medicaid and CHIP programs can use MCQ oversight activities to inform and support QI projects.
- Using State Managed Care Quality Strategies for Quality Improvement in Medicaid and CHIP (video, slides). This video describes QS elements and how states can use the QS for QI projects.
- Using Managed Care External Quality Review for Quality Improvement in Medicaid and CHIP (video, slides). This video describes EQR, EQR-related activities, and the use of EQR recommendations and findings for QI projects.
- NEW: Quality Improvement in Medicaid and CHIP Managed Care: Quality Assessment and Performance Improvement (QAPI) Programs (video, slides, transcript). This 2026 webinar describes QAPI programs and how states can use QAPI for QI in Medicaid and CHIP.
- COMING SOON: QAPI Progress Report Template. This resource provides a template states can use to monitor plans’ QAPI programs. Please email ManagedCareQualityTA@cms.hhs.gov for a Word version of the template.
Technical assistance is available. Please submit any questions or requests for technical assistance related to MCQ improvement to ManagedCareQualityTA@cms.hhs.gov

