Technical Instruction History
| Date | Description of Change |
|---|---|
06/27/2022 |
Original technical instructions issued |
08/04/2022 |
|
09/08/2022 |
The compliance date for the instructions pertaining to sub-capitated encounter records and provider file data was changed from “one year after the date of publication of these technical instructions” to July 1, 2023. |
11/19/2024 |
Technical instructions updated to align with T-MSIS Data Dictionary V4.0.0
|
Brief Issue Description
This technical instruction document identifies the challenges states have faced when reporting payments by managed care plans to sub-capitated entities (referred to as “sub-capitation payments” below) for the management or provision of specific enrollee services as well as the associated encounter records for the services provided. The state T-MSIS technical instructions below explain how to report sub-capitation payments, the associated sub-capitated encounter records, and sub-capitated provider affiliation to T-MSIS, including the T-MSIS file to which they should be mapped and how key data elements should be populated.
Background Discussion
Context
States frequently contract with managed care plans to manage and ensure the delivery of care to Medicaid, Medicaid-expansion Children’s Health Insurance Program (M-CHIP), and separate Children’s Health Insurance Program (S-CHIP) program enrollees. In turn, these managed care plans can contract with other entities to facilitate the delivery of a specific set of services to a specific set of enrollees. These entities can include other managed care plans, administrative services organizations, subcontractors[1], or network providers.[2] These entities contracted with managed care plans are considered “sub-capitated entities” if they receive periodic payment regardless of the scope, duration, or volume of services a particular enrollee receives during the period covered by the payment (i.e., they are paid on an at-risk basis).
For example, a managed care plan could contract with a dental pre-paid ambulatory health plan (PAHP) and pay that PAHP a pre-defined sub-capitation payment for each person enrolled in the PAHP in a given month. Because the PAHP is at risk, the sub-capitation payment would be paid to the PAHP regardless of whether the enrollee received any services in that month.
In contrast, claim payments that managed care plans make to providers that are paid for each service rendered (e.g., fee-for-service payments) are not considered sub-capitated. For example, if a managed care plan contracts with a dental PAHP on a non-risk basis to provide services and the amount of the payment made by the managed care plan to the dental PAHP is always paid per-service, then the dental network is not considered a sub-capitated entity. Managed care plans may also establish agreements with network providers, either individuals or large organizations, to deliver services to beneficiaries in exchange for a periodic payment that is not directly contingent on the specific scope, duration, or volume of services provided to a particular beneficiary during the period covered by the payment (i.e., they are paid on an at-risk basis).
Definitions
- The term “Medicaid and S-CHIP agencies” (see Figure 1) is used to mean either the unit or units of state government that administer(s) Medicaid and/or S-CHIP. Medicaid expansion CHIP (M-CHIP) is administered by the Medicaid agency. For the purposes of these technical instructions, the term ‘Medicaid’ will include M-CHIP, unless otherwise specified.
- The terms “managed care plan” (see Figure 1) and “MCP” are used to refer to the managed care plans that have a direct contract with the state Medicaid and/or S-CHIP agencies. In accordance with 42 CFR 438.2, managed care plan types include: comprehensive managed care organization (MCOs), prepaid inpatient health plans (PIHPs), prepaid ambulatory health plans (PAHPs), and primary care case management (PCCM) entities.
- Per 42 CFR 438.2, the term “network provider” (see Figure 1) means any provider, group of providers, or entity that has a network provider agreement with a MCO, PIHP, or PAHP, or a subcontractor, and receives Medicaid funding directly or indirectly to order, refer, or render covered services as a result of the state's contract with an MCO, PIHP, or PAHP. There are two types of network provider: 1) a capitated network provider and 2) a sub-capitated network provider. A capitated network provider is one that is not paid on a fee-for-service basis but is also not sub-contracted to the managed care plan because the managed care plan and the network provided are really one in the same. A sub-capitated network provider is sub-contracted to either a managed care plan or sub-capitated entity.
- The term “subcontractor” or “subcontracted entity” refers to an individual or entity that has a contract with an MCO, PIHP, PAHP, or PCCM entity that relates directly or indirectly to the performance of the MCO's, PIHP's, PAHP's, or PCCM entity's obligations under its contract with the State. A network provider is not a subcontractor by virtue of the network provider agreement with the MCO, PIHP, or PAHP.
- The term “capitation payment” (see Figure 1) refers to the payments that state Medicaid or S-CHIP agencies make to managed care plans to cover contracted services. The term “sub-capitation payment” refers to the payment from the managed care plan to the sub-capitated entity or sub-capitated network provider to cover contracted services on an at-risk basis.
- There are two types of sub-capitated arrangements: 1) a sub-capitated entity arrangement and 2) a sub-capitated network provider arrangement.
- “Sub-capitated entity” (see Figure 1) refers to an entity that the managed care plan contracts with to facilitate the delivery of and pay providers for contracted services in exchange for a sub-capitation payment. The sub-capitated entity uses the sub-capitation payments to reimburse rendering providers. Sub-capitated arrangements should generate managed care encounters; the sub-capitated entity must report the encounter data to the managed care plan so that the managed care plan can, in turn, report the sub-capitated encounter to the state Medicaid or S-CHIP agency. Because sub-capitated entities receive sub-capitated payments from managed care plans regardless of services rendered, the actual dollar value of the services on sub-capitated encounter records associated with a given enrollee will not necessarily equal the sub-capitation payment(s) for that enrollee. A sub-capitated entity is a type of “sub-contracted entity”.
- “Sub-capitated network provider” (see Figure 1) refers specifically to a network provider that a managed care plan contracts with to render contracted services in exchange for a sub-capitation-payment. Because the sub-capitated network provider is the rendering provider, there would not be a fee-for-service payment amount to report on the service utilization records that become sub-capitated encounters when reported to the state Medicaid or S-CHIP agency by the managed care plan.
- The term “managed care encounter” refers to the information relating to the receipt of any items(s) or service(s) by an enrollee under a contract between a state and a MCP. There are two types of managed care encounters submitted to T-MSIS:
- Capitated encounter records (see Figure 1) for which the rendering provider was paid on a fee-for-service basis by the managed care plan or an administrative-services only subcontractor of the managed care plan, and
- Sub-capitated encounter records (see Figure 1) for which a sub-capitated entity was paid a sub-capitation payment from the managed care plan. This second type of encounter is one of the areas of focus of this guidance.
- There are two types of sub-capitated encounter records:
- Sub-capitated encounter records from providers who are paid by the sub-capitated entity on a fee-for-service basis (see Figure 1).
- Sub-capitated encounter records from sub-capitated network providers (see Figure 1)
Figure 1. Payment and Data Relationships Between State Medicaid/S-CHIP Agency, Network Providers, Managed Care Plans, Sub-Capitated Entities, and Sub-capitated Network Providers
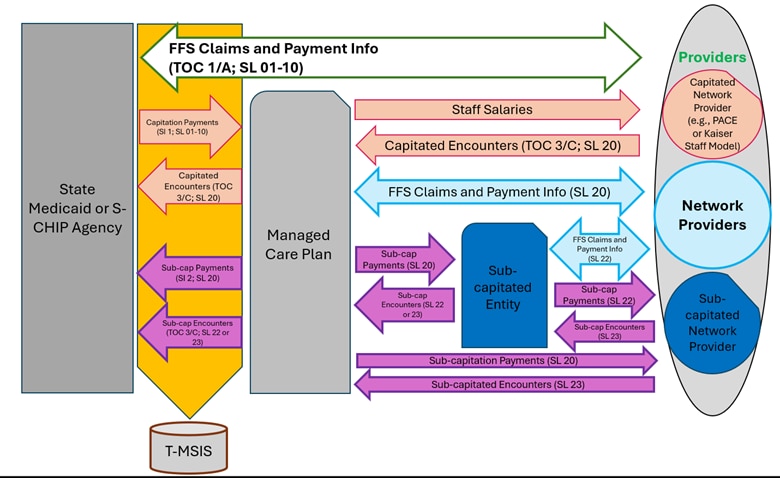
TOC= TYPE-OF-CLAIM (OT, IP, LT, RX)
SI= SUBCAPITATION-INDICATOR (FTX)
SL= SOURCE-LOCATION (FTX, OT, IP, LT, RX)
Note: In the v4 File Layout, capitations and sub-capitations are reported to the FTX00002 (INDIVIDUAL-CAPITATION-PMPM) segment.
Note: SL values for capitations, sub-capitations, and encounters between the Managed Care Plan, the Sub-capitated Entity, and Providers are included in the figure for awareness.
Challenge
States have faced challenges when attempting to report sub-capitation payments and the associated sub-capitated encounters in their T-MSIS files because there has been no way to distinguish between capitation payments versus sub-capitation payments and capitated encounters versus sub-capitated encounters. Sub-capitated arrangements make up an increasing share of services within Medicaid. States must report in T-MSIS files all services covered by their Medicaid program and S-CHIP, including those services (captured on sub-capitated encounters) paid for with sub-capitation payments.
Capitation payments from state Medicaid and S-CHIP agencies to their contracted managed care plans are directly matched by federal dollars, but dollars paid out by the managed care plan (both sub-capitation payments and FFS claim payments) are not. Therefore, failure to distinguish sub-capitation payments from managed care plans and capitation payments from state Medicaid and S-CHIP agencies in the T-MSIS submissions would cause Medicaid and S-CHIP expenditures to be overstated.[3] As a result, only capitation payments from state Medicaid and S-CHIP agencies have historically been reported in T-MSIS to avoid any misinterpretation.
Likewise, states and T-MSIS data users have run into challenges with distinguishing between capitated encounter records and sub-capitated encounter records in T-MSIS. In particular, Medicaid and S-CHIP agencies have inquired about how to report to T-MSIS payment-related data elements on some types of sub-capitated encounter records, including payment-related reporting for sub-capitated network provider encounters.
Technical Instructions
The technical instructions below provide information on how sub-capitation payments and sub-capitated encounter records should be reported in T-MSIS. The first two sections detail the technical instructions on reporting sub-capitated encounter records for sub-capitated entities and sub-capitated network providers. The third section provides technical instructions on reporting sub-capitation payments. The fourth section provides technical instructions on reporting sub-capitated network provider information on the managed care file.
Reporting Sub-capitated Encounter Records from Sub-capitated Entities to T-MSIS
Sub-capitated encounter records collected by managed care plan from their sub-capitated entities should be reported to all applicable T-MSIS claims file types (i.e., CIP, CLT, COT, and CRX). Sub-capitated encounter records should be reported with the existing TYPE-OF-CLAIM (CIP100, CLT052, CRX029, COT037) valid values of “3” for Medicaid and Medicaid-expansion CHIP enrollees and TYPE-OF-CLAIM value of “C” for S-CHIP enrollees (see Table 1).
Table 1 - Sub-capitated Encounter Data Elements with Reporting Clarifications [4]
| Date Element Number | Data Element Name | Reporting Instructions Based on Whom Submitted the Encounter to the MCP: Sub-capitated Entity | Reporting Instructions Based on Whom Submitted the Encounter to the MCP: Sub-capitated Network Provider |
|---|---|---|---|
CIP100 |
TYPE-OF-CLAIM |
For sub-capitated encounters from a sub-capitated entity, report TYPE-OF-CLAIM = "3" for a Medicaid sub-capitated encounter record or “C” for an S-CHIP sub-capitated encounter record. |
For sub-capitated encounters from a sub-capitated network provider, report TYPE-OF-CLAIM = "3" for a Medicaid sub-capitated encounter record or “C” for an S-CHIP sub-capitated encounter record. |
CIP112 |
TOT-BILLED-AMT |
For sub-capitated encounters from a sub-capitated entity that is not a sub-capitated network provider, report the total amount that the provider billed the sub-capitated entity for the service. Report a null value in this field if the provider is a sub-capitated network provider. |
For sub-capitated encounters from a sub-capitated network provider, if the sub-capitated network provider directly employs the provider that renders the service to the enrollee, report a null value in this field. |
CIP113 |
TOT-ALLOWED-AMT |
For sub-capitated encounters from a sub-capitated entity that is not a sub-capitated network provider, report the total amount that the sub-capitated entity allowed for the service. Report a null value in this field if the provider is a sub-capitated network provider. |
For sub-capitated encounters from a sub-capitated network provider, if the sub-capitated network provider directly employs the provider that renders the service to the enrollee, report a null value in this field. |
CIP114 |
TOT-MEDICAID-PAID-AMT |
For sub-capitated encounters from a sub-capitated entity that is not a sub-capitated network provider, report the total amount that the sub-capitated entity paid the provider for the service. Report a null value in this field if the provider is a sub-capitated network provider. |
For sub-capitated encounters from a sub-capitated network provider, if the sub-capitated network provider directly employs the provider that renders the service to the enrollee, report a null value in this field. |
CIP104 |
SOURCE-LOCATION |
For sub-capitated encounters from a sub-capitated entity that is not a sub-capitated network provider, report a SOURCE-LOCATION = "22" to indicate that the sub-capitated entity paid a provider for the service to the enrollee on a FFS basis. |
For sub-capitated encounters from a sub-capitated network provider, report a SOURCE-LOCATION = “23” to indicate that the sub-capitated network provider provided the service directly to the enrollee. |
CIP130 |
PLAN-ID-NUMBER |
For sub-capitated encounters from a sub-capitated entity, report the PLAN-ID-NUMBER for the MCP (MCO, PIHP, or PAHP that has a contract with a state) that is making the payment to the sub-capitated entity. |
For sub-capitated encounters from a sub-capitated network provider, report the PLAN-ID-NUMBER for the MCP (MCO, PIHP, or PAHP that has a contract with a state) that is making the payment to the sub-capitated network provider. |
COT174 |
BILLED-AMT |
For sub-capitated encounters from a sub-capitated entity that is not a sub-capitated network provider, report the amount that the provider billed the sub-capitated entity at the claim line detail level. Report a null value in this field if the provider is a sub-capitated network provider. |
For sub-capitated encounters from a sub-capitated network provider, if the sub-capitated network provider directly employs the provider that renders the service to the enrollee, report a null value in this field. |
CIP251 |
REVENUE-CHARGE |
For sub-capitated encounters from a sub-capitated entity that is not a sub-capitated network provider, report the amount that the provider billed the sub-capitated entity at the claim line detail level. Report a null value in this field if the provider is a sub-capitated network provider. |
For sub-capitated encounters from a sub-capitated network provider, if the sub-capitated network provider directly employs the provider that renders the service to the enrollee, report a null value in this field. |
CIP252 |
ALLOWED-AMT |
For sub-capitated encounters from a sub-capitated entity that is not a sub-capitated network provider, report the amount that the sub-capitated entity allowed at the claim line detail level. Report a null value in this field if the provider is a sub-capitated network provider. |
For sub-capitated encounters from a sub-capitated network provider, if the sub-capitated network provider directly employs the provider that renders the service to the enrollee, report a null value in this field. |
CIP254 |
MEDICAID-PAID-AMT |
For sub-capitated encounters from a sub-capitated entity that is not a sub-capitated network provider, report the amount that the sub-capitated entity paid the provider at the claim line detail level. Report a null value in this field if the provider is a sub-capitated network provider. |
For sub-capitated encounters from a sub-capitated network provider, if the sub-capitated network provider directly employs the provider that renders the service to the enrollee, report a null value in this field. |
The SOURCE-LOCATION (CIP104, CLT056, COT041, CRX032) field is used to distinguish between a provider who was ultimately paid by the managed care plan, a sub-capitated network provider, or any other sub-capitated entity. If the managed care plan pays a provider directly for Medicaid/S-CHIP enrollee’s service(s) on a FFS basis, then the SOURCE-LOCATION data element should be reported with a value of “20”. If the sub-capitated entity pays a provider for the Medicaid/S-CHIP enrollee’s service on a FFS basis, then the SOURCE-LOCATION data element should be reported with the new valid value of “22”. Accurately reporting the SOURCE-LOCATION data element allows data users to accurately identify which managed care encounters should be reported with payment information.
Finally, the PLAN-ID-NUMBER (CIP130, CLT080, COT066, CRX056) field on the sub-capitated encounter record should be reported with the managed care plan identifier for the managed care plan that issues the payment to the sub-capitated entity and contracts directly with the Medicaid or S-CHIP agency. All other data elements reported on sub-capitated encounter records should be reported consistently with the claims file reporting requirements noted in the data dictionary. If a field can be reported on a managed care encounter record, then the same information should be reported on a sub-capitated encounter record.
The compliance date for reporting sub-capitated encounter records from sub-capitated entities to T-MSIS is July 1, 2023.
Reporting Sub-Capitated Encounter Records from Sub-capitated Network Providers to T-MSIS
In some situations, the sub-capitated entity is a network provider that provides services directly to an enrollee. In these cases, the sub-capitation payment directly covers the services for the enrollee and the sub-capitated entity does not pay for services on a fee-for-service basis. Under this scenario, the billed amount, the revenue charge amount, allowed amount, and the paid amount fields should all be reported with a null value and the SOURCE-LOCATION data element should be reported with the new valid value of “23”. TYPE-OF-CLAIM and PLAN-ID-NUMBER and all other data elements applicable to managed care encounters are treated the same for encounters from sub-capitated entities, sub-capitated network providers, and capitated network providers. Table 1 above summarizes the technical instructions for sub-capitated encounter record data elements that have updated reporting requirements for encounters from sub-capitated network providers.
The compliance date for reporting sub-capitated encounter records from sub-capitated network providers to T-MSIS is July 1, 2023.
Reporting Sub-capitation Payments
As of the T-MSIS Data Dictionary V4.0.0, capitation and sub-capitation payments should now be reported on the FTX00002 segment of the Financial Transactions file type, consistent with the reporting requirements identified in the T-MSIS data dictionary and the T-MSIS data dictionary appendices. All capitation payments should be reported with valid date values in the PAYMENT-OR-RECOUPMENT-DATE, CAPITATION-PERIOD-START-DATE, and CAPITATION-PERIOD-END-DATE. Most data elements reported for sub-capitation payments should be populated in the same way they would be for a state-to-managed care plan capitation payment with the exception of the data elements identified in the following paragraphs. This applies to sub-capitation payments made to sub-capitated entities and sub-capitated network providers.
Sub-capitation records should be reported with SUBCAPITATION-IND (FTX056) value of “2” for the sub-capitation payment. These records should also be reported with SOURCE-LOCATION (FTX054) value of “20” to capture financial transactions between a managed care plan and an entity that is not the state Medicaid or CHIP agency. This value indicates that the source of the payment is the managed care plan. These transactions include sub-capitation payments to sub-capitated entities and sub-capitated network providers. States should also report a PAYER-ID-TYPE (FTX029) value of “02” to represent the plan.
Additionally, the PAYER-ID (FTX028) reported on the sub-capitation payment should be populated with the unique T-MSIS plan identifier for the managed care plan that is issuing or recouping the payment (and is contracted with the state Medicaid/S-CHIP agency). It is important that the sub-capitated entity or sub-capitated network providers with whom a managed care plan has a contract should not be identified as a managed care plan on the T-MSIS managed care file, as the Managed Care File only captures plans that contract directly with the Medicaid or CHIP agency. Instead, this entity or network provider should be identified as a provider using the PAYEE-ID (FTX033) field on the sub-capitation payment record and either the SUBMITTING-STATE-PROV-ID (PRV019, PRV042, PRV063, PRV075, PRV087, PRV097, PRV109, PRV118, and PRV128) or PROV-IDENTIFIER (PRV081) on the T-MSIS provider file. The PAYEE-ID-TYPE (FTX034) value of “04” should be used on the sub-capitation payment record, representing the sub-capitated network provider ID. If the sub-capitated network provider does not have an NPI, then the entity should be documented in the same way that an atypical provider would be documented.
This document lays out a summary of key data elements for reporting sub-capitation payments in T-MSIS files. All other data elements reported on sub-capitation payment records should be reported consistently with the FTX file reporting requirements noted in the data dictionary. If a field can be reported on a capitation payment record, then the same information should be reported on a sub-capitation payment record.
The compliance date established for reporting sub-capitation payments to T-MSIS has not yet been determined.
Reporting sub-capitated network providers on the Provider File
The relationship between the MCP and its sub-capitated network providers should be clearly identified on the T-MSIS provider file. A sub-capitated network provider should be uniquely identified on the PROV-AFFILIATED-PROGRAMS-PRV00009 segment of the provider file using AFFILIATED-PROGRAM-TYPE (PRV119) value of “6” to indicate that it is sub-capitated network provider and should be reported with the managed care plan ID that pays that network provider sub-capitation payments.
Each individual provider and facility that is owned or employed by the sub-capitated network provider should be reported with a PROV-AFFILIATED-GROUPS-PRV00008 segment to identify the relationship between the provider and the sub-capitated network provider. The SUBMITTING-STATE-PROV-ID of the PROV-AFFILIATED-GROUPS-PRV00008 segment would belong to the owned or employed provider and the SUBMITTING-STATE-PROV-ID-OF-AFFILIATED-ENTITY would belong to the sub-capitated network provider to show that each provider is owned or employed by the sub-capitated network provider.
For example, in table 3 below, the sub-capitated network provider Universal Health Providers (SUBMITTING-STATE-PROV-ID -OF-AFFILIATED-ENTITY = 4) is a sub-capitated network provider with three employed providers, Dr. One, Dr. Two, and Dr. Three (SUBMITTING-STATE-PROV-ID = 1, 2, and 3 respectively). The three records for Dr. One, Dr. Two, and Dr. Three are reported with a SUBMITTING-STATE-PROV-ID (PRV109) value of “1”, “2”, and “3” on each respective record, and the SUBMITTING-STATE-PROV-ID-OF-AFFILIATED-ENTITY (PRV110) is populated with a value of “4” on all three records. These three records show that each of the three providers is employed by Universal Health Providers Network.
Sub-capitated network providers should otherwise be reported with the same types of information as those expected for providers that directly contract with a managed care plan that holds a contract with a state Medicaid or S-CHIP agency.
Table 3 - Affiliated Provider Group Reporting
| SUBMITTING-STATE-PROV-ID | SUBMITTING-STATE-PROV-ID-OF-AFFILIATED-ENTITY | PROV-AFFILIATED-GROUP-EFF-DATE | PROV-AFFILIATED-GROUP-END-DATE |
|---|---|---|---|
| 1 | 4 | 10/01/2019 | 12/31/9999 |
| 2 | 4 | 10/01/2019 | 12/31/9999 |
| 3 | 4 | 10/01/2019 | 12/31/9999 |
The compliance date for identifying sub-capitated network providers on the provider file is July 1, 2023.
Summary
When applicable, states must be able to distinguish between capitation payments, capitated encounters, sub-capitation payments, and sub-capitated encounters in their T-MSIS file submissions so that CMS can properly interpret and analyze them, particularly the sub-capitation payments. To facilitate states’ ability to make this distinction, CMS introduced a new file segment for reporting capitations and sub-capitation payments in the T-MSIS Data Dictionary v4.0. Additionally, CMS previously introduced two new SOURCE-LOCATION values to identify sub-capitated encounters (‘22’ if the provider was ultimately paid for the encounter by a sub-capitated entity, ‘23’ if the provider was ultimately paid for the encounter by a sub-capitated network provider), and one new AFFILIATED-PROGRAM-TYPE for sub-capitated network providers (‘6’). The compliance date for the instructions pertaining to sub-capitated encounter records and provider file data was July 1, 2023. The compliance date for the instructions pertaining to sub-capitation payments has not yet been determined.
Endnotes
[1] Defined at 42 CFR 438.2
[2] Defined at 42 CFR 438.2
[3] This distinction is part of the reason why Medicaid FFS claims, S-CHIP FFS claims, Medicaid encounters, and S-CHIP encounters are reported with different TYPE-OF-CLAIM values.
[4] States should refer to the most recent version of the T-MSIS Data Dictionary for technical instructions on reporting other data elements.
 An official website of the United States government
An official website of the United States government

